The world is changing. As we grapple with the escalating impacts of climate change, those of us in the healthcare sector stand at a crucial crossroads. We see evidence of increasing frequency and intensity of climate-related events — like heatwaves, wildfires, floods, and infectious disease outbreaks — and we know they pose significant threats to public health and vulnerable populations. Health systems are on the front lines and are the first responders to climate emergencies so they must continually adapt to these challenges, leverage innovations to mitigate their own emissions, and spearhead efforts toward building a more climate-resilient industry that can deliver effective, uninterrupted care.
Climate resilience is the ability of a people, group, or ecosystem to bounce back after a hazardous climate event like a flood, drought, or emergencies caused by storms and related disease outbreaks. The healthcare industry plays an important role in stabilizing our ability to recover and make positive changes.
Climate mitigation is the action of limiting the emissions of greenhouse gases in the atmosphere to help avoid the worst impact of climate change. The healthcare industry accounts for 8.5% of U.S.-based greenhouse gases (GHGs). Concurrently, industry leaders are hearing increased calls to their responsibility to lead by example and cut emissions while building climate-resilient health systems.
With resource-intensive operations and rising accompanying costs, health systems need to look at decarbonization efforts to transition from energy- and resource-intensive consumption models to climate-smart interventions that reduce utility consumption, provide energy independence, integrate smart purchasing models, view life cycle costs, and reduce carbon footprints to cut costs that can be holistically reinvested into health systems.
By integrating sustainable practices and climate-smart strategies, healthcare institutions can mitigate the health repercussions of a changing climate, improve the strength of their organizations, safeguard our communities, and ensure a healthier future for all.
The Impact of Climate Change on Our Health
The CDC lists a variety of documented outcomes associated with our changing climate, including:
- Increased heat-related hospital visits for respiratory issues
- Rising number of heat-related cardiovascular and kidney disorders
- Higher exposure to mold, food, and water-borne illnesses from flooding
- Higher incidences of asthma due to increased air pollution
- Increased pollen and higher allergy rates related to longer growing seasons
- Increased wildfire activity, resulting in more cases of asthma and COPD from poor air quality
- Higher incidences of poor mental health following climate-related disasters
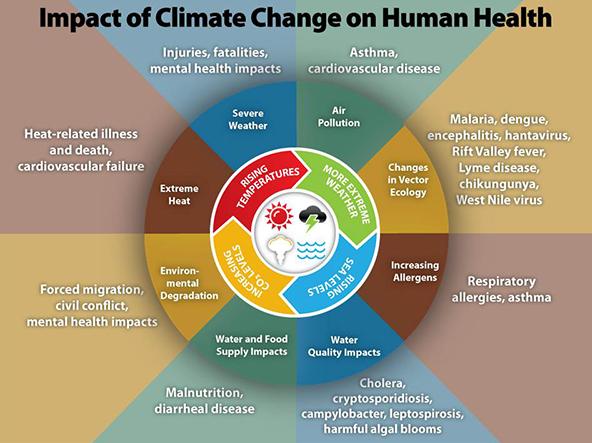
According to the World Health Organization (WHO), weather and climate hazards directly and indirectly impact people’s health. The Lancet Countdown provides hope that, even though climate change is a staggering threat, it also offers a great opportunity to redefine those things that have such a negative impact. The healthcare industry can — and should — lead efforts toward action and meet the growing calls to do its part in alleviating climate change.
The Healthcare Industry and Greenhouse Gases
First, we acknowledged that the healthcare industry accounts for 8.5% of U.S.-based GHGs, but the industry has become more, not less, polluting. Emissions increased 6% between 2010 and 2018. Healthcare facilities and operations are incredibly climate intensive, impacting the environment and public health significantly. These GHG emissions come from various sources within the health sector:
Energy Consumption
Hospitals, clinics, and laboratories are energy-intensive facilities that require substantial energy for ventilation systems, lighting, and running specialized medical equipment. Many healthcare facilities are located in geographies that rely on local fossil fuel-based energy sources, such as coal, natural gas, and oil, which emit high levels of GHGs.
The increasing use of digital health records and the growth of data centers require robust IT infrastructure, which consumes large amounts of electricity.
Medical Equipment and Devices
Most of the emissions for a health system are embedded in their indirect Scope 3 emissions from the production and transportation of goods and services procured. The production of important medical devices and equipment involves energy- and resource-intensive processes that emit greenhouse gases throughout the life cycle. Some medical equipment also uses climate-intensive gases, such as nitrous oxide or desflurane, as anesthetics and hydrofluorocarbons (HFCs) in refrigeration — which are potent greenhouse gases that persist in the atmosphere.
Building Construction and Maintenance
Building new sustainable healthcare facilities or renovating existing ones involves massive amounts of embedded carbon within material inputs and construction processes. The extraction, production, transportation, and installation of building materials and the operational and end-of-life phases of a healthcare facility also contribute substantially to emissions.
Medical Waste
Medical waste is often incinerated to prevent contamination, and this incineration process releases carbon dioxide and other harmful gases. Organic waste that decomposes in landfills produces methane, a potent GHG. These facilities are also often located in disenfranchised areas, with local communities bearing the brunt of negative health impacts.
Transportation
Hospital fleet vehicles, ambulances, helicopters, and other medical transport vehicles contribute significantly to GHGs. The production and transportation of medical supplies, food, and other necessary goods for healthcare facilities involve emissions at various stages, from manufacturing to delivery. Staff commuting and business travel also contribute to emissions and offer opportunities for reductions.
Crucial Steps Toward Reduced Emissions
There is much work to be done, and commitments are required on numerous fronts. In an effort to accelerate industry progress on decarbonization and health equity, the U.S. Department of Health and Human Services launched the Health Sector Climate Pledge in 2022, with voluntary commitments to do the following:
- Reduce organizational emissions 50% by 2030 and achieve net zero emissions by 2050.
- Designate an executive level lead to work on reducing emissions by 2023 and conduct an inventory of Scope 3 (supply chain/indirect emissions) by the end of 2024, or within 6 months of signing the pledge.
- Release a climate resilience plan for continuous operations by the end of 2023 or within six months of signing the pledge.
Additionally, within the past year both the Joint Commission and the Centers for Medicare and Medicaid Services (CMS) released voluntary climate reporting standards and certifications for hospitals and health systems. More broadly, the Securities and Exchange Commission and the state of California passed mandatory climate disclosure and reporting rules. These rapid increases in voluntary climate related commitments and mandatory disclosures is sending a strong signal that healthcare entities need to strategically prioritize decarbonization related efforts to meet growing stakeholder expectations.
Changing the Story: Climate Resilience and Mitigation for Better Health Outcomes
The goal of healthcare institutions is to improve health, not damage it. So, we must change the story, executing proven climate mitigation interventions and reductions that can save millions in related costs, while creating climate resilience–ready infrastructure and facility systems that deliver positive health outcomes for patients. Effective strategies are already helping leading healthcare institutions reduce their negative climate impact and save substantial costs. The business case is undeniable. These strategies simultaneously help clinics, hospitals, and healthcare centers positively impact their bottom line through extensive savings and improve the health of the stakeholders they serve.
This ROI of climate action benefits both the hospital and the community by:
- Improving energy efficiency, saving costs, and protecting against rising utility rates
- Adopting renewable energy sources and creating energy independence
- Meeting increased stakeholder and regulatory demands
- Preserving population and community health
- Enhancing supply chain efficiencies and resilience
- Improving waste management practices
- Encouraging sustainable transportation options
The other lens can be seen as the emergent ROI of climate action or the “risk of inaction.” The major risk is an interruption in patient care and operations due to extreme weather, disruption of critical supply chains, rising health inequities, and revenue losses. The human risks are all too real and the business risks are rising by the day.
Oakwell offers robust and comprehensive help for healthcare institutions to assess where change needs to happen, create important goals, and then implement measures with roadmaps tailored to complement current operations in reducing the environmental impact of patient care delivery. We’ve seen vast reductions in calculated emissions of the institutions we work with and significant improvements to their companies’ bottom lines that only compound over time.
We are helping healthcare systems improve profitability by focusing on climate change sustainability and acting as stewards of their resources. We help our partner institutions discover extensive energy and utility cost savings, optimize real estate assets, create more efficient supply chain logistics, reduce waste generation, and reduce the overall climate impacts of their daily healthcare operations.
Leading the Way With Sustainable Healthcare
As healthcare leaders, we hear the call to take responsibility for addressing the factors in operations that lead to poor health outcomes for the populations we serve and making the changes necessary for truly sustainable care delivery. The healthcare industry’s goal is to improve the health of the communities we serve, and Oakwell is here to improve the health of your system and those you serve.
Oakwell has realized the extensive positive impact on the bottom line of the sustainable healthcare systems we’ve partnered with. But just as important is the positive impact on the communities they serve, with reduced healthcare costs, improved public health, and increased preparedness for rising climate-related events. And taking proactive action toward climate resilience and mitigation is a win-win for everyone, with long-term ripple effects. We can help you strengthen your community engagement and brand recognition, further building trust with patients, staff, and your community.
Our diverse team of experts in hospital operations, sustainability, engineering, technology, and finance has figured out how to improve the sustainability of your healthcare system and save you money doing it. We partner with you every step of the way toward decarbonization and resiliency. We will help you quantify and track your Scope 1, 2, and 3 climate impacts, create strategic goals, tailor master plans, and work collaboratively to implement the necessary changes via dedicated roadmaps and direct resources for the desired outcomes. We will stay with you after implementation to help you measure and verify those changes in real time and make necessary adjustments.
Oakwell will create organizational functions that help you act as stewards of resources within your health system and improve your bottom line. Let’s work together to create a healthier future for your healthcare system and our planet.

